Being self-insured, do you cringe every time you send one of your injured workers to the emergency room or occupational medicine clinic?
This case study illustrates how you can manage this expense while increasing access to qualified providers.
Case Study
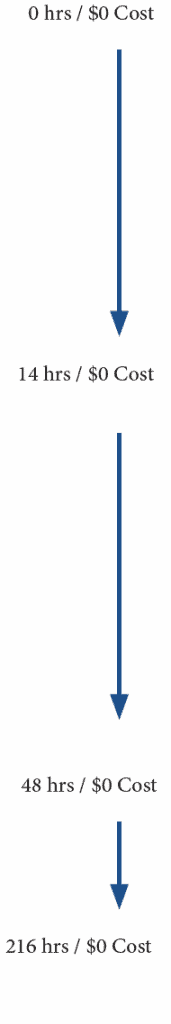
On a SATURDAY MORNING, the on-call provider was notified of an employee that had an injury that may need to go to the emergency room or have a virtual workers comp clinic visit.
A video consult was immediately performed, and it was felt the patient needed anti-inflammatory pain medication and a shoulder sling. The medication was electronically prescribed, she was instructed on how to get the sling and work status was determined.
EARLY THE NEXT MORNING AT APPROXIMATELY 1:30 AM, the patient notified the on-call provider that her pain was up to 9/10. The provider performed another virtual consult and learned that that the patient had not picked up the prescription or the sling. In fact, she had been using her arm in a way that exacerbated her pain.
The patient was reminded of the treatment plan and instructed to ice the area. She assured the provider that she would pick up the prescription and the sling. She was told she could come to the clinic for an in-person visit at any time.
TWO DAYS LATER, she did come into the clinic for her first in-person exam. Her pain level at that time was down to 2/10.
ONE WEEK LATER, a follow-up consult was performed, and she had no pain and was released.

• The company had a direct contract with the clinic, which provided access to the on-call provider 24/7
• The injured worker had immediate access to a provider
• Up to two emergency room visits were avoided
• An appropriate treatment plan was provided, which included medication
Discussion
Through direct contracting with the clinic, the employer was able to handle this injury on a pre-claim basis and at a fixed cost.
“Workers’ compensation is more like a finance tool than an insurance policy. Ultimately, through the experience modification, you will pay for your actual claims. The only way to lower the cost of workers’ compensation, in the long run, is to lower the frequency and severity of the claims that are driving those costs.”
Cavignac Construction Newsletter
So, if an employer can pay for work injuries on a pre-claim basis, it makes great financial sense to do so.
The concept of direct contracting with a clinic introduces a refreshing new approach to healthcare and how it is paid for. Through the Direct Primary Care (DPC) model, physicians are “uncoupled” from the Fee for Service (FFS), system that requires them to try to link everything they do to something that is reimbursable by a third party (the insurance company).
85 % of total workplace injuries in 2006 and 2017 were caused by overexertion, contact with objects or equipment or falls, slips, and trips. (**https://www.ncci.com/Articles/Documents/Insights-WorkforceDemographics.pdf)
Conclusion
Since most work injuries are minor injuries, they can be handled through the virtual work comp clinic at a fixed cost.
If a hands-on visit is required, it can be done at a reasonably contracted rate between the clinic and the company. In this way, the employer is not losing control of the cost of the injury by sending the injured worker into a system that is designed to make money by looking for any reimbursable charge they can find.



Recent Comments