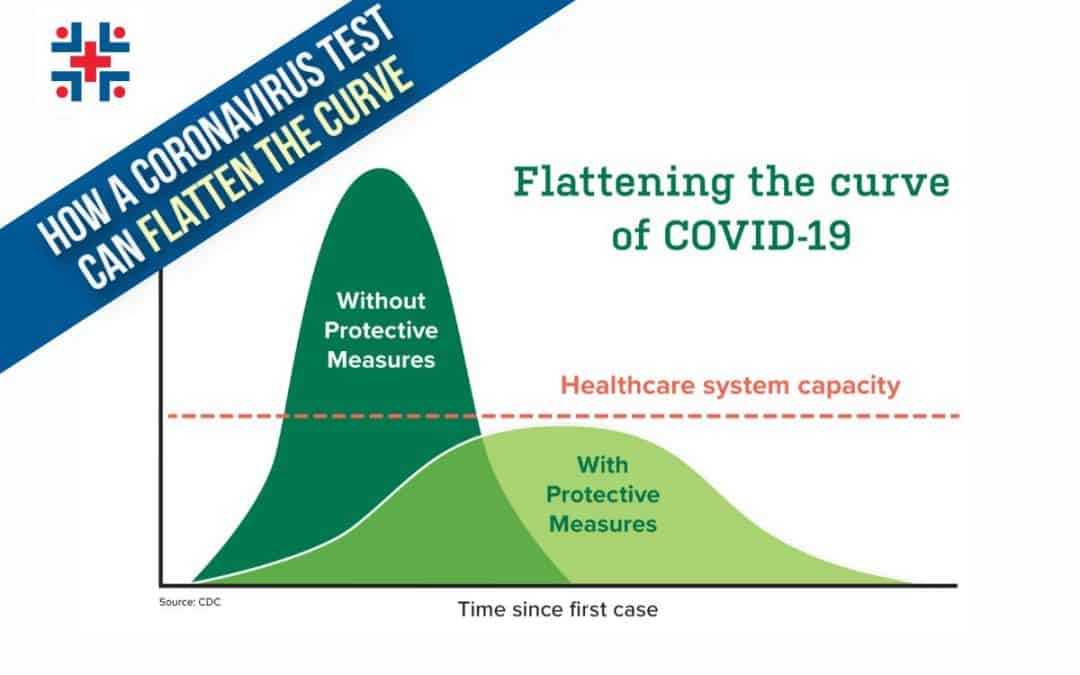
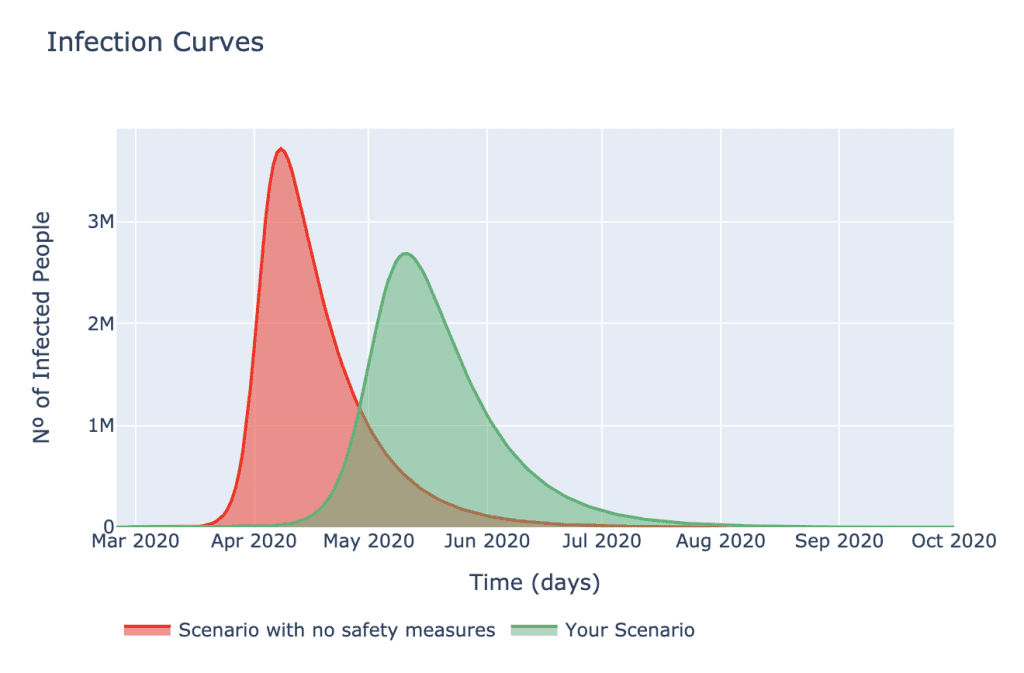
The longer it takes to slow the spread of Coronavirus or COVID 19, the greater outcome of hospitalizations, Intensive Care Unit admissions, and death. Smart, aggressive universal testing in combination with the practice of social distancing, good hygiene and Stay Home Work Safe measures can help to flatten the curve and save lives.
Coronavirus Outbreak
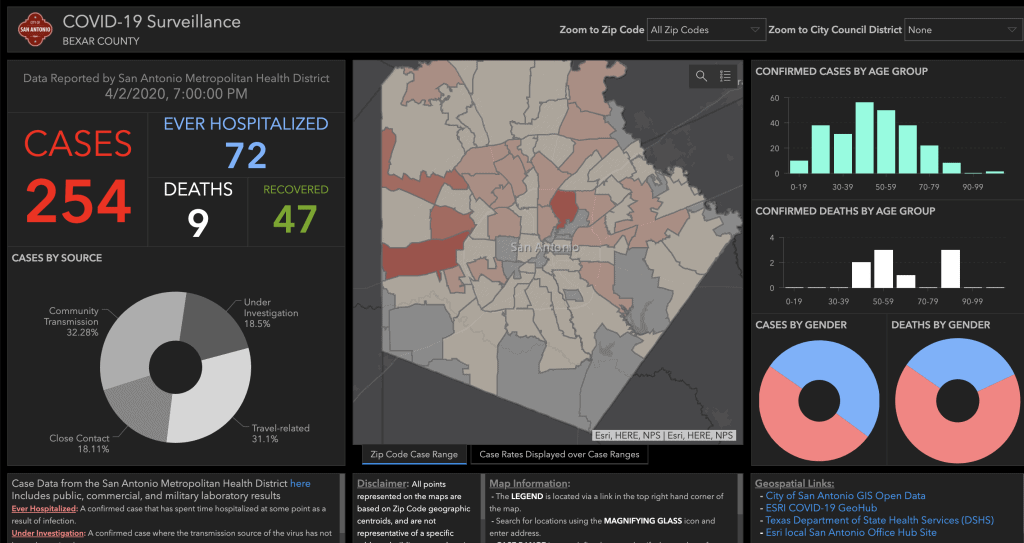
In December 2019, there was a cluster of pneumonia cases in China that brought alarm to the international community. The WHO named the virus Severe Acute Respiratory Syndrome or SARS CoV-2 as responsible for leading to this potentially fatal infection of the lungs, which we now refer to as COronaVIrus Disease 2019 or COVID-19. The outbreak has now swept into other parts of the globe becoming a pandemic killing more than 50,000 and going.There has now been community spread to Bexar County, Texas, with about ⅓ of the 207 cases occurring through community transmission. Community spread means people are becoming infected and do not know-how. Community spread is unrelated to recent travel of the outbreak or close contact with someone who is a known carrier of the disease.
What Does Flatten the Curve Mean?
To flatten the curve is to slow the spread of infection to a rate that does not exceed the healthcare system capacity. State and local authorities, the WHO, CDC and others are suggesting recommendations to slow the spread which include social distancing, practicing good hygiene and Stay Home Work Safe measures. But will it work?
a. Social Distancing means to avoid crowds that are larger than a recommended number. At present, meetings larger than 10 are discouraged. Elderly and immunocompromised individuals should stay home. An immunocompromised person is someone with a weakened immune system and includes people with heart disease, lung disease, kidney disease, diabetes, HIV/AIDS, cancer and transplant patients.
b. Practicing good hygieneis essential to eliminating the chances of the virus’s spread and survival on high-touch surfaces.
Hand hygiene
- Wash hands with soap and water regularly for 20 seconds after:
- Food handling (before/during/after)
- Blowing nose
- Caring for sick
- Treating a cut or wound
- Using the bathroom
- Touching animals
- Touching garbage
Dry hands to prevent germs.
- Avoid touching nose, mouth, and eyes.
- Use 60% alcohol-based hand sanitizer if soap and water are not available.
- Avoid high-touch surfaces.
Respiratory hygiene
- Clean high-touch surfaces in case infected droplets land there
- Cough or sneeze in the elbow and throw tissue away in a closed canister.
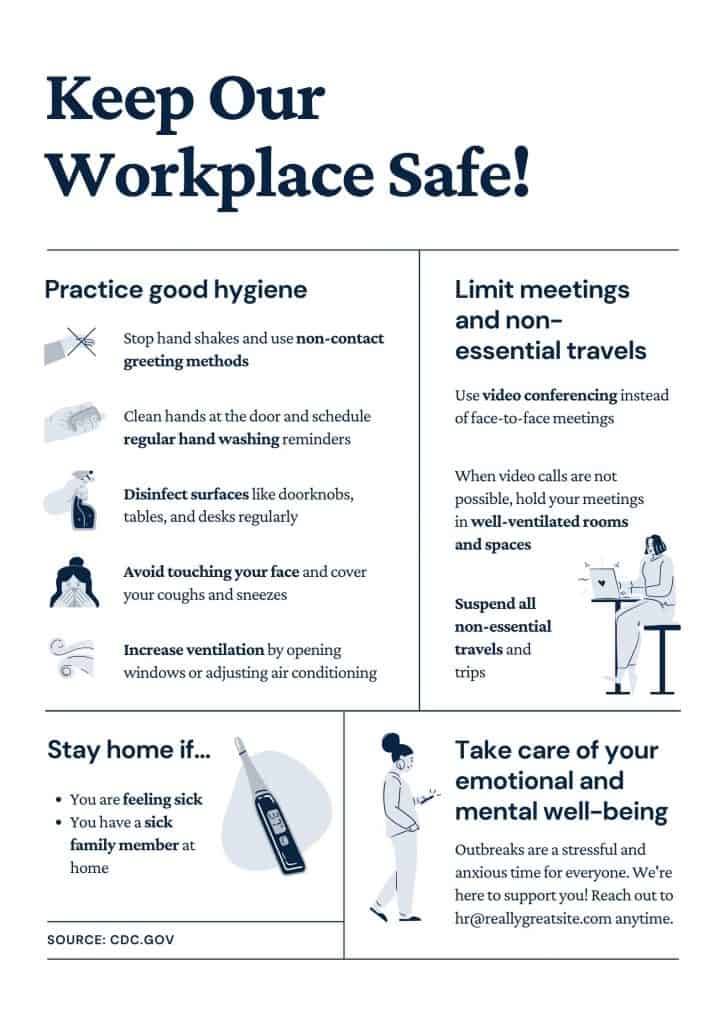
c. Stay Home Work Safe Measures
The Stay Home Work Safe measures encourage isolation and quarantine in order to keep the city safe. Practicing social distance puts space between silent carriers of the disease as well as self-isolation and quarantine.
Isolation is separation between people who are sick with the virus from people who are not sick.
Quarantine takes isolation a step further by placing separation between those exposed and not exposed through movement restrictions to determine who is infected. These may come in the form of suggested guidelines, state or local orders. Quarantine is extremely powerful as it prevents asymptomatic individuals from transmitting the disease.
Texas Healthcare System Capacity
Despite all of the precautions put into place through social distancing, practicing good hygiene and Stay Home Work Safe measures, there are still barriers to care and hurdles for Texans to overcome that will put a strain on the healthcare system. These barriers to care relate to lack of physical access, insurance and a critical shortage of care. Those who will need access to care to treat serious cases of COVID-19 will have varying levels of difficulty depending on these barriers.
Access
Texas has the highest number of rural hospital closures (20) in the country. According to the Texas Department of Agriculture, 64 Texas counties do not have a hospital and there are on average 35 miles between critical access. Some Texans must travel 100 miles to reach the nearest hospital. “The first 60 minutes after a trauma or cardiac event could mean the difference between life and death,” Texas Department of Agriculture Commissioner Sid Miller. This leaves rural Texas vulnerable.
Insurance
Unfortunately, Texas ranks #1 in number and percentage of uninsured individuals compared to the rest of the United States. 5 million Texans are uninsured, especially Hispanics/Latinos, younger people, and those who fall 200% under the poverty line. Of the Texans who are insured, most are still underinsured, meaning that, relative to their income, their deductibles and out-of-pocket expenses are still too high. Coronavirus hospitalization can cost uninsured Americans an estimated average of $73,300 for a 6-day hospital stay, according to a recent report by FAIR Health. Texans who can physically reach a facility for hospitalization will unlikely be able to take the financial hit.
Shortage of Care
75% of Texas counties are federally designated Health Professional Shortage Area (HPSA) and/or Medically Underserved Area (MUA). Even if Texans manage to overcome most of the barriers preventing them access to care, the literal shortage of doctors and nurses means that many Texans will go without critical care if the Texas healthcare system collapses. 25 counties in Texas do not have primary care physicians, meaning patients who are delaying care for fear of costs or lack of coverage will flood the emergency room and urgent care centers instead of referring to their doctor. According to Texas DSHS, Texas only has 8,826 intensive care beds, far less than what will be needed in the weeks to come, and this includes the number of beds that are unavailable. When the flood critically enters these facilities, medical professionals will be unprepared, as Texas medical professionals also face a shortage of supplies. Following the national pattern, Texas is short on hand sanitizer, facial masks, respirators, ventilators and PPE, posing a serious threat.

Underlying health conditions
In addition to deferring care until the situation becomes emergent, every year, diabetic amputations rise. The percentage of adults in San Antonio diagnosed with type 1 or 2 diabetes increases every year, as over 14% of San Antonio adults have diabetes, according to the DSHS. San Antonio’s rate is higher than the Texas average of 10%, which is slightly higher than the national average of 9%, according to the CDC.

With a high prevalence of diabetes and obesity steadily increasing, San Antonio becomes a vulnerable community at risk for more COVID-19 related complications which will lead to a high number of deaths. Even with all of the precautions to flatten the curve, San Antonio needs more solutions to prevent COVID 19 sickness and death.
“In a COVID-19 outbreak on a cruise ship where nearly all passengers and staff were screened for SARS-CoV-2, approximately 17 percent of the population on board tested positive as of February 20; about half of the 619 confirmed COVID-19 cases were asymptomatic at the time of diagnosis.”
Coronavirus disease 2019 (COVID-19)

This highlights the importance of testing as a solution. Smart, aggressive testing with a 15-minute antibody test combined with the practice of social distancing, good hygiene, and Stay Home Work Safe measures can help to flatten the curve and save lives.

Recent Comments