How Much Does Chronic Disease Cost Businesses?
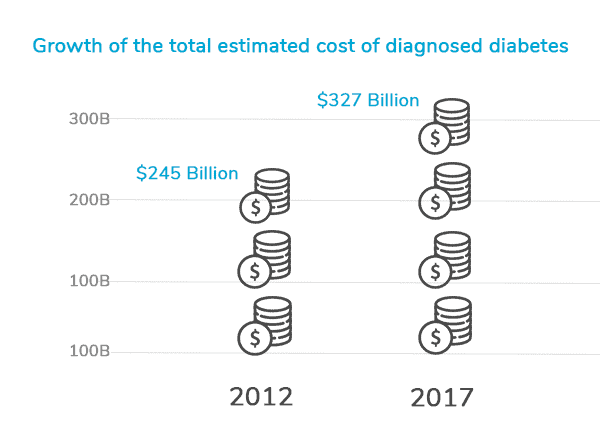
Employers need high-performing primary care with chronic disease self-management programs and support for their employees. Highly-trained health care professionals who use preventive care can help patients to manage their chronic conditions with long-lasting strategies and a sensible health plan that actually produces results. Journal articles in such places as PMC free article or recent studies found in Cochrane Database of Systematic Reviews, for example, have shown that preventative care helps to better patient outcomes and lower health care costs (Disease Management Interventions For Heart Failure). Robust studies such as the Milliman Study, evaluate models of care such as Direct Primary Care, show a new healthcare model of delivery and financing, through a market study completed by 200 DPC physicians. This is great to examine not only the quality of care for patients but the cost effectiveness for employers who adopt this model of care. Assessing disease-specific clinical outcomes also helps to monitor improvements in health and finances compared to traditional care delivery system.
Primary care providers need to be at the center of the conversation to improve health outcomes with collaborative care in combination with disease management programs. This is why we have created the Doctor’s Program, a program that is not centered around insurance, but around the doctor-patient relationship in order to get the best primary care management and chronic disease care a patient deserves that won’t break the employer’s bank. A primary care provider should be a regular part of population health management. With health IT tools, telemedicine and virtual care mobile tools like the HIPAA compliant app that Direct Med Clinic provides, providers can track improvement in outcomes of a patient and help with generic medications to care coordination. Staying directly connected in the chronic disease self-management program with primary care professionals is what contributes to a high quality experience for our patients and also what distinguishes this direct primary care from conventional care.
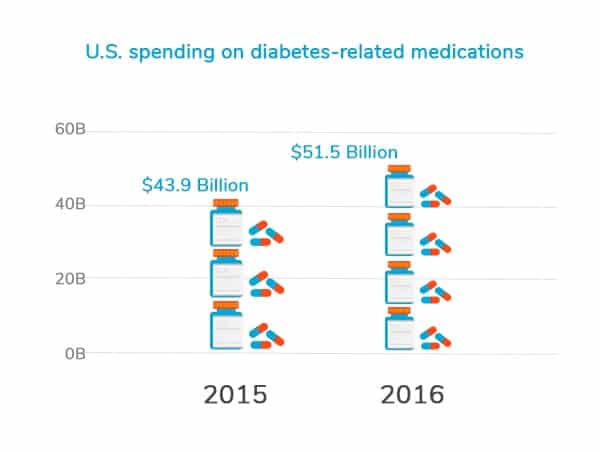
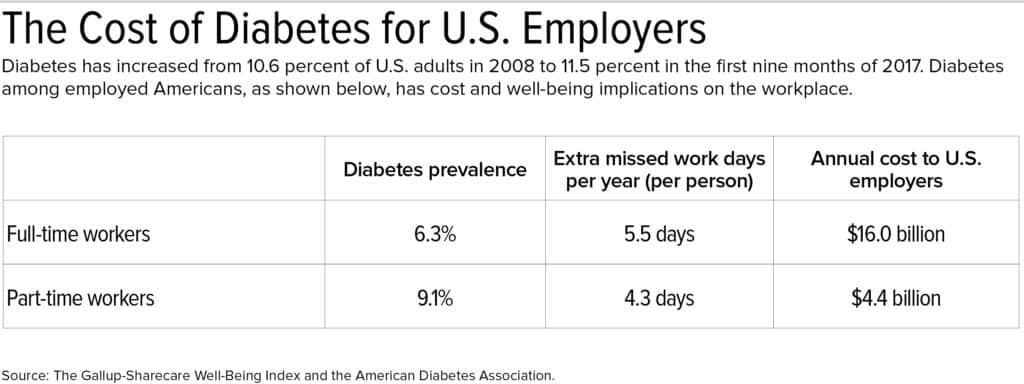
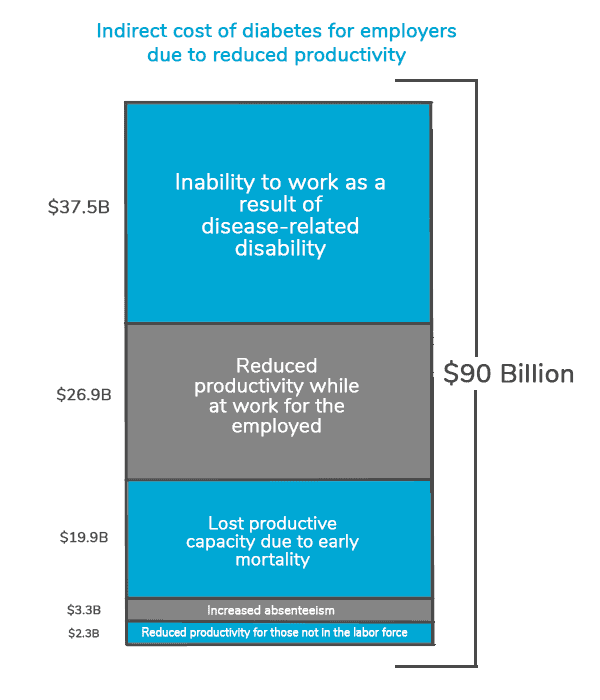
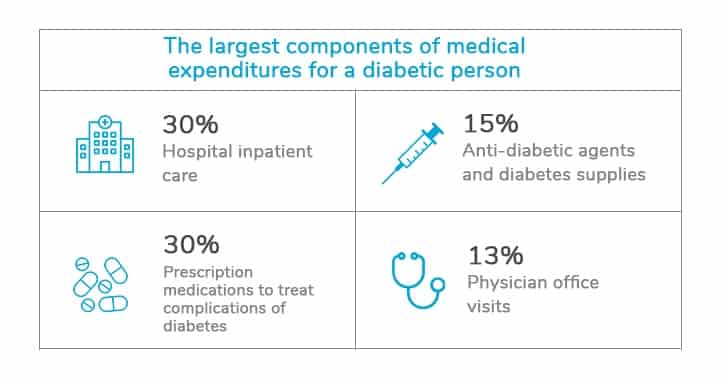
Our Direct Primary Care healthcare delivery model can be thought of as a chronic care model that progressively provides improvements in outcomes and helps to save on downstream costs. Chronic care management programs have been known to reduce the burden of disease and keep healthcare costs down. Direct Med Clinic’s healthcare delivery system design naturally takes care of chronic heart failure, cardiovascular diseases, diabetes care, chronic health condition, long-term conditions, heart disease, pulmonary disease. However, regular access to health care is required for disease management programs by health care providers who are trained to provide health services and a form of care conducive to adult patients with diabetes mellitus and other chronic illnesses. This is one of the best ways to increase inventory due to improved worker productivity. A Chronic Disease Management Program should deliver more clinical effectiveness and better patient outcomes and is not just another wellness program.
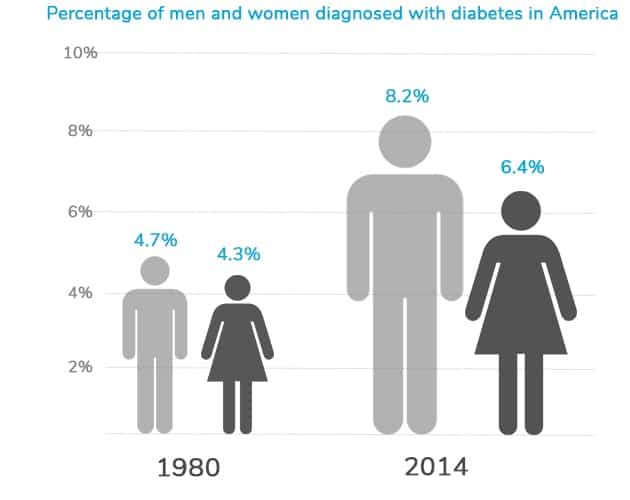
In 2013, San Antonio implemented intentional community health pathways for diabetes. Although there are community-based programs with some community resources for disease management patients, the continuity of care from the care managers and the accessibility to healthcare providers matters greatly. They need to be able to evaluate their medication quality, patient level outcomes, monitor improvements in outcomes, tracking the category of outcome, and comparing to usual care. These programs help individuals and families make better decisions about their daily health, but a primary care health professional can help with self-management support regularly. Nevertheless, it is good to partner with health systems that allow for the social care of our communities. An intentional community health approach focuses on preventive and curative interventions. They improve the physical and mental well-being of people living in a community. Individuals, their adults, and children with chronic conditions, diabetes, some cancers, high cholesterol, and arthritis can all benefit from community-based interventions. When individuals manage their health, it will decrease the long-term costs. An oral diabetes educator teaches oral care skills, and is a fantastic educator, for example.
We need to focus on prevention, assess, and manage these conditions together. Bexar County is not alone. In some states, less than 10% of the counties have an employee-funded healthcare provider of any kind, such as Montana and Wyoming. We must think of ways to help our employees get the care they need, while also supporting local healthcare providers and incorporating different healthcare stakeholders. In other words, affordable healthcare should be considered a stage in the prevention and management of chronic conditions as a primary element and direct the given care model decision.
Chronic diseases should not all be treated by specialists, but managed by healthcare professionals, and paid for by employers at a cost and a way that does not deplete their financial resources. Bexar County’s uninsured rate is 45% and climbing. Access to healthcare has been declining because of rising costs. Despite working with companies who are strapped for cash, the best outcomes are reserved for those companies with both rich employer support and a well-connected workforce.
Working with self-management and prevention tools like these requires partnership and collaboration with providers, payers, insurance companies, employers, and public programs. Direct Med Clinic offers it all. Our health initiatives focus on diabetes management, preventative care, and wellness. We work with people with no health insurance to develop an affordable lifestyle to afford preventive and curative health care. We empower people with diabetes to become educated and take care of themselves and their well-being. We offer community support, education, and advocacy to guide individuals in their care for diabetes and other underlying health conditions management. We have a program where people with lost or aneurysms, traumatic brain injury, and kidney disease can get service coordination and education. Bexar County will continue to set ambitious goals. The San Antonio community will set unique goals. And Direct Med Clinic will use Direct Primary Care to work together to strive for a better tomorrow with direct, accessible, transparent, and affordable care.
Contact us for stronger designs in your population health management with a customized chronic disease self-management program for your employees.


Recent Comments